Vaginoplasty – laparoscopically assisted peritoneal pull through
Reconstruction of the neovagina is of utmost importance in transfemales. It is sometimes the first, but sometimes the last surgery performed in an individual’s transition.
So far, the gold standard in neovaginal creation for transfemales is considered penile inversion vaginoplasty with long-term very good and satisfying results in many centers around the world. Bowel vaginoplasty was considered in cases where penile and scrotal skin were inadequate for satisfying vulvovaginal complex reconstruction or for cases of RE-DO surgeries.
During the last decade, an old technique, introduced by Russian gynecologist Davydov, came into light in gender affirming surgeries as another possibility for vaginal lining.
The surgery can be offered as a primary vagioplasty in transwomen, or if possible for RE-DO cases.
The surgery is performed in general anesthesia. The patient is positioned in an exaggerated lithotomy position. Complete penectomy is performed until the attachments of the corpora cavernosa to the pubic bones, bilateral orchiectomy in known fashion, and cavity, between the urethra, bladder and rectum is created for vaginal lining. Using 3 ports and pneumoperitoneum, camera is introduced into the cavity, and mobilization of the peritoneal flaps is performed from the bladder and urethra above, and from rectum below, and anastomosis with the skin flaps is made inside the channel. In this way additional depth of the vagina is secured as well as natural lubrication (at certain level).
Vulvoplasty (clitoris, labia and urethra) is done like in penile inversion vaginoplasty.
The vaginal packing is placed inside the vagina with antibiotic ointment for 7 days and urinary catheter as well for 12 days postoperatively.
The dilation of the neovagina is commenced after vaginal packing removal, according to the instructions given by the therapist and should be performed for at least 12 months in regular fashion (twice a day for 45 minutes) Vaginal flushing is advised in terms of removal of the lubricant gel from the neovagina.
CASE 1 – Surgical procedure

Preoperative appearance
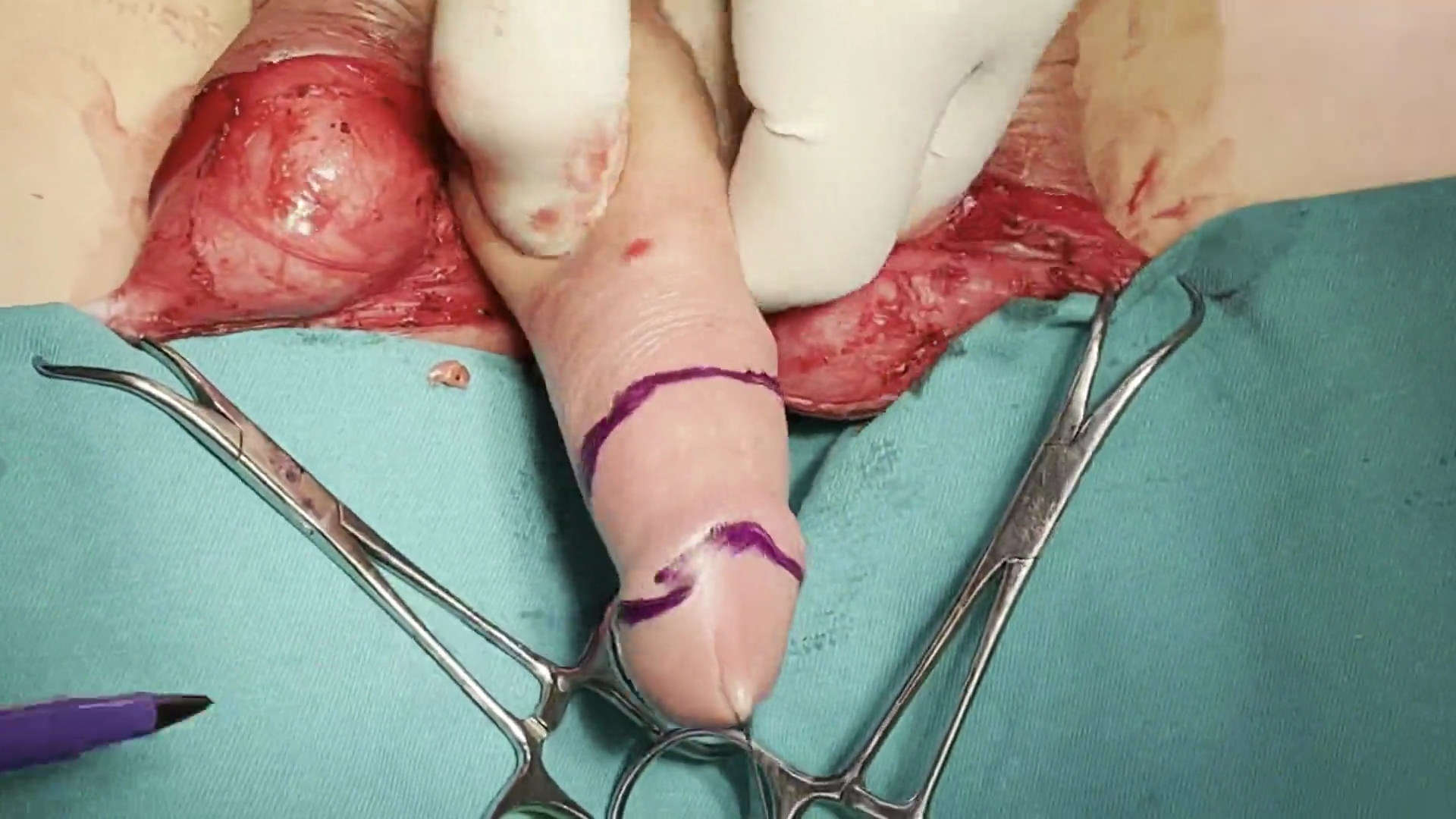
Design of the neoclitoris and labia minora
Penile disassembly. Dissection of urethra ventrally and neurovascular bundle dorsally
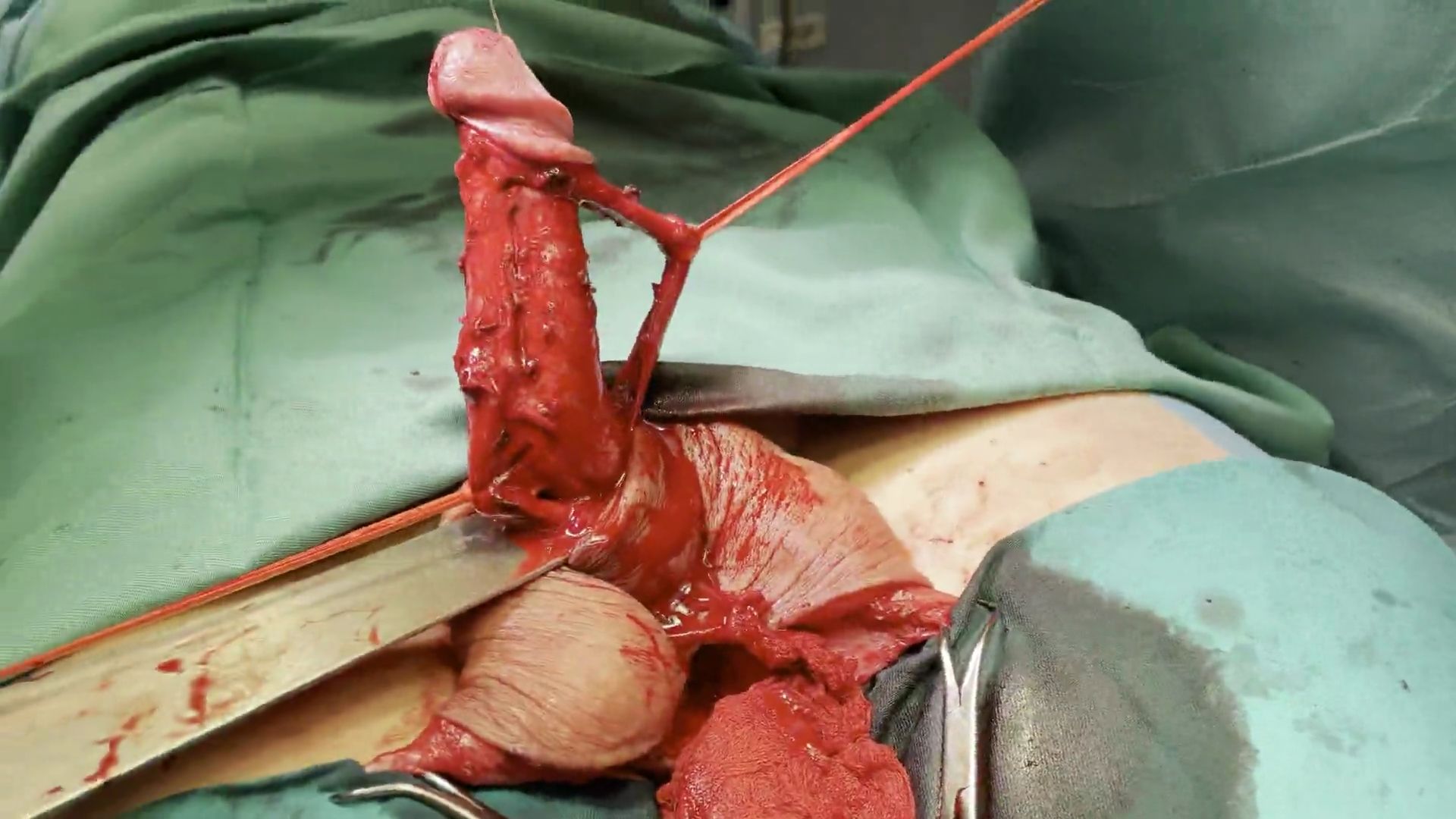
Total penectomy is performed. Cavernosal bodies are removed to the level of the attachment to the pubic bone.
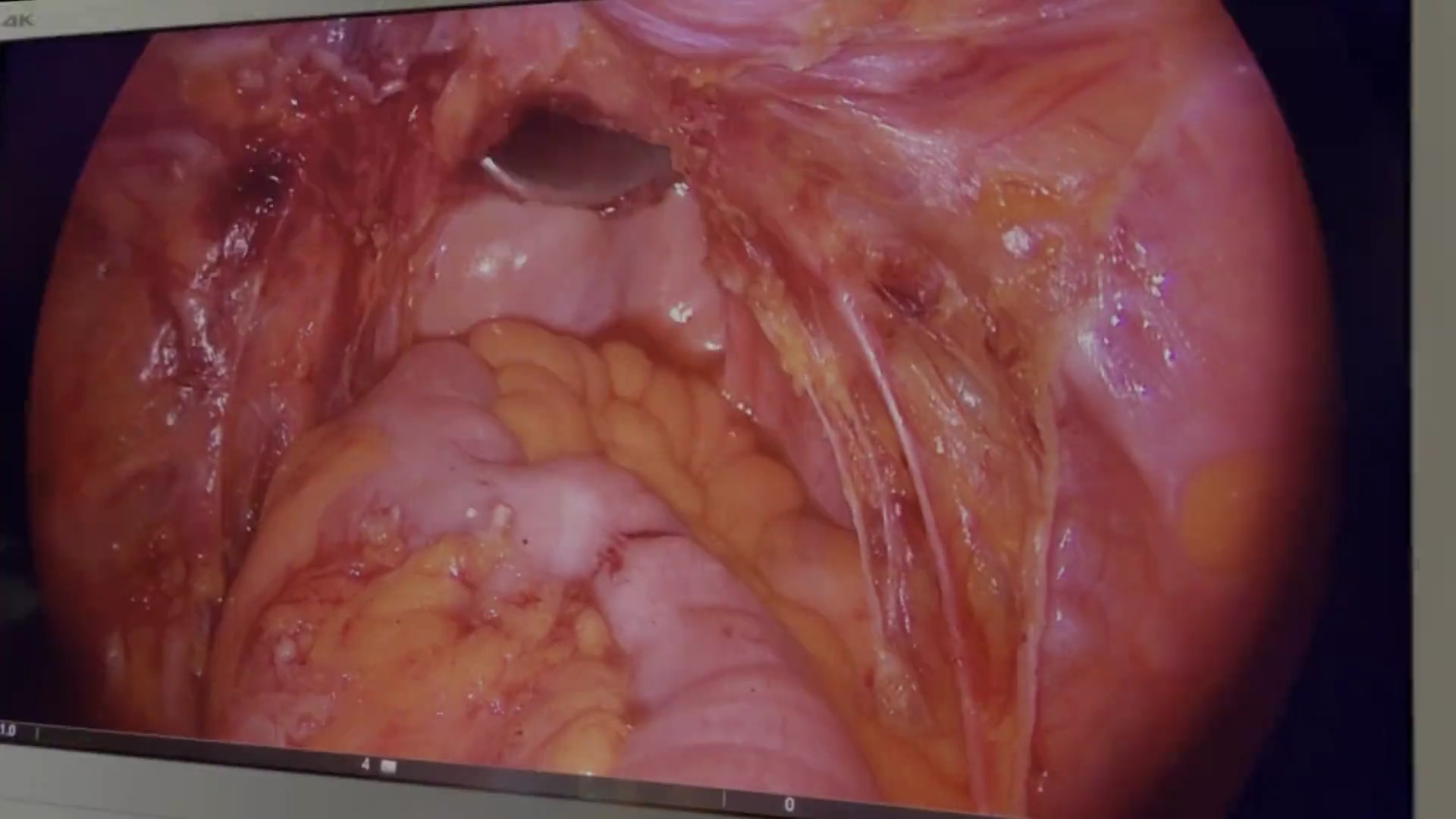
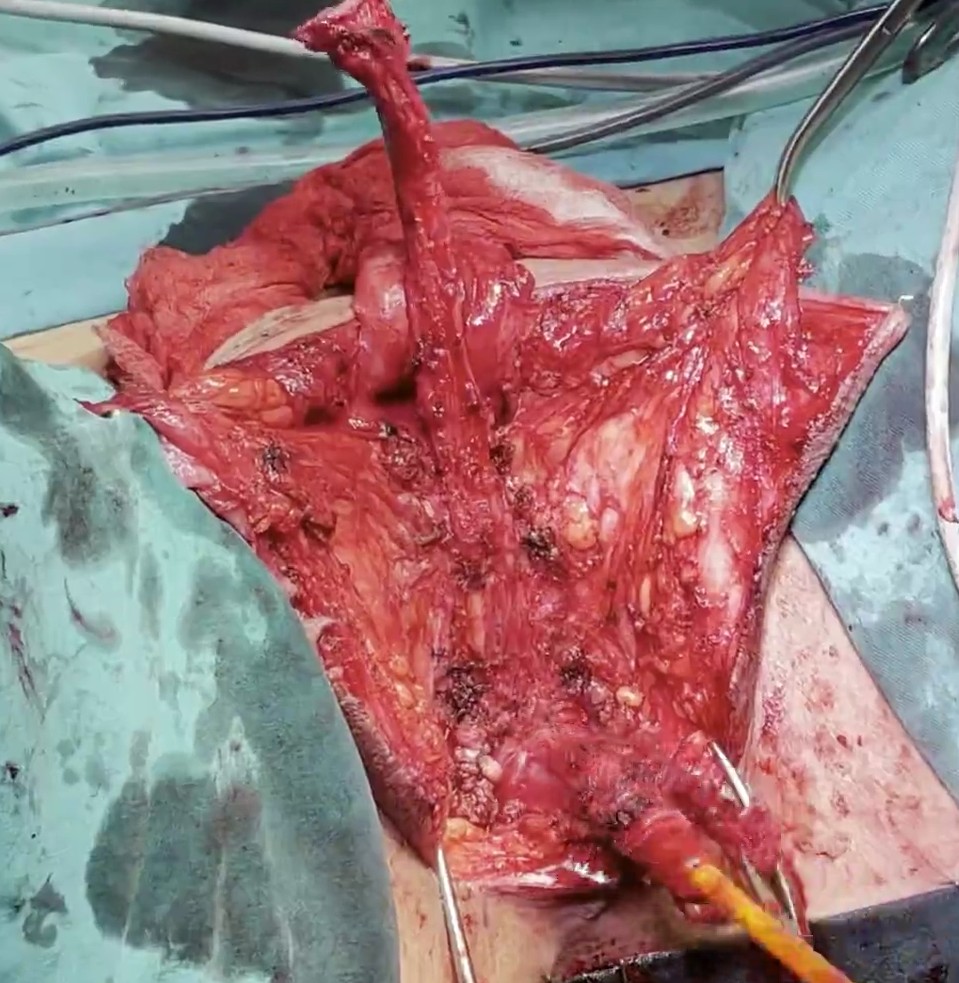
Peritoneal flaps are created using laparoscopic approach. Space for the neovagina is created between the bladder and the rectum, and retractor is placed.

Peritoneal flaps are anastomosed with inverted penile skin using perineal approch, to create neovagina.
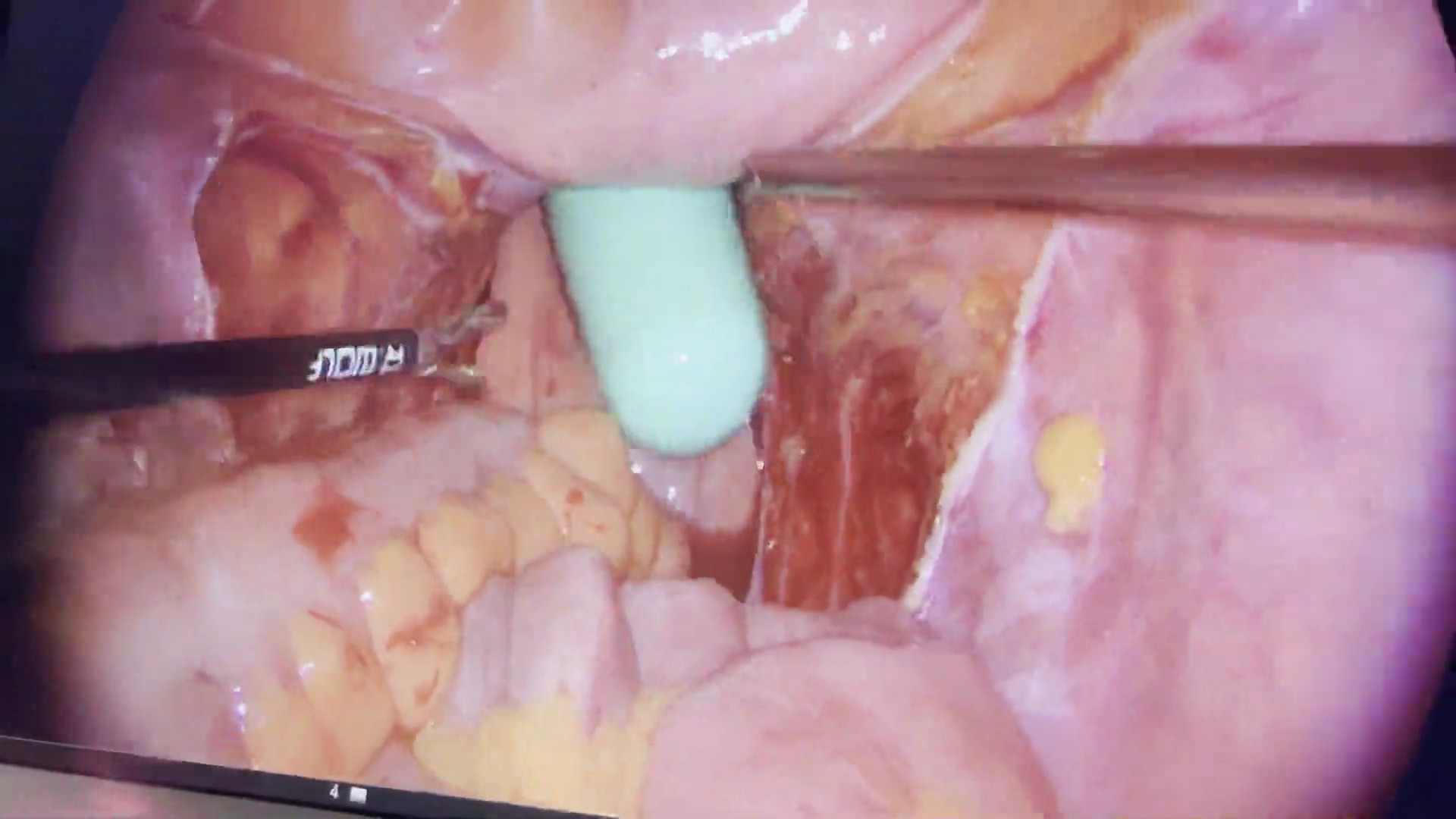
Dilator is placed into the abdominal part of the neovagina.
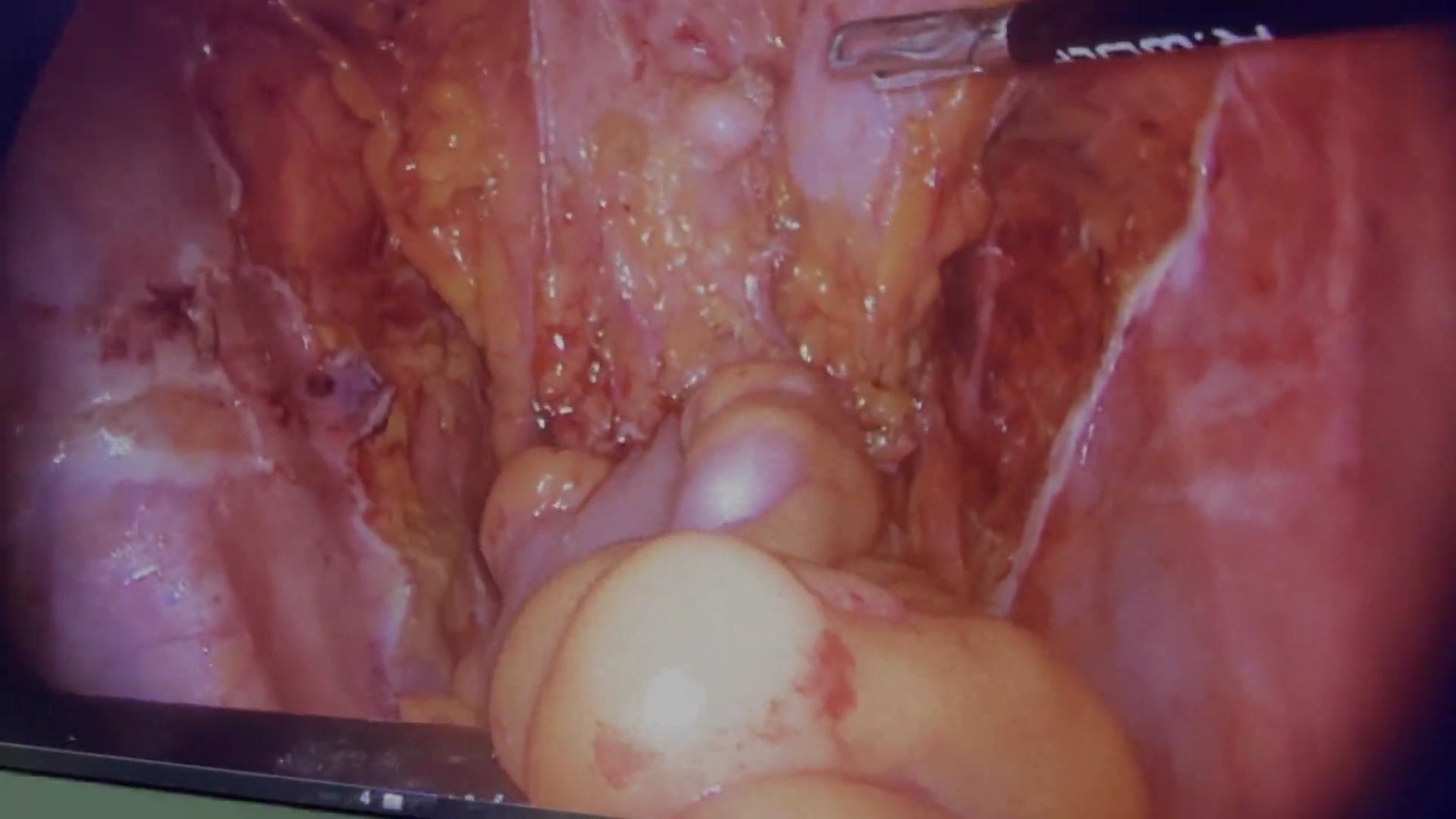
Proximal part of the neovagina is closed over the dilator.

Result after surgery. Neovagina has excellent depth.

Outcome 3 weeks after surgery. Good depth of the neovagina is achieved.
CASE 2
Result 7 days after vaginoplasty


CASE 3
Result after 7 days. Good depth of the neovagina.

CASE 4
Outcome one month after vaginoplasty.


CASE 5
Outcome 3 months after vaginoplasty.

CASE 6
Outcome 6 months after vaginoplasty.
