Penile enhancement
Development of female cosmetic surgery followed by rising popularity of reconstructive genital surgery induced that penile lengthening and widening gained tremendous interest in male population. Considerable improvement of penile aesthetic appearance and size is now possible, although this surgery remains a challenge requiring strict attention and ethical evaluation.
Treatment
Various methods were employed in recent years for penile girth extension, resulting in many postoperative complications and disappointing outcome. The most common method, lipofilling, results in deformities such as asymmetry of the penis or curvature, as well as irregular distribution of fat nodules. Silicone liquid injection also has been used commonly for cosmetic purposes in recent years, primarily to fill small defects. It is not recommended due to many complications including migration, swelling, penile deformities and late granulomatous reactions. Corporeal body enlargement can also be achieved by expanding the tunica albuginea with saphenous vein graft, but there are deficient reports to confirm the reliability and efficacy of this procedure. Tissue engineering brought a revolution in penile enhancement surgery with fabricating a new functional tissue from autologous cells. A great success in penile girth enlargement was achieved using biodegradable scaffolds (poly-lactic-co-glycolic acid, PLGA) as a carrier for autologous cells. However, production of PLGA scaffolds was shut down, which made us to search for new and better solutions.
This is why we introduced autologous dermal fat grafting as the method of choice for penile girth enhancement. The principle is to use patient’s own fatty tissue taken from gluteal region, and place it under the penile skin, in circumferential manner, for penile augmentation. This technique has numerous advantages: the procedure is safe, minimally invasive, and can be performed in regional anesthesia; donor site scar remains hidden under the gluteal groove; there is no risk of rejection since the patient’s own tissue is used; fast recovery and return to normal activities in 4-6 weeks.
Technique
Gluteal region is shaved preoperatively. Physical measurements of penile length and mid-shaft penile circumference both in the flaccid and erect state are obtained and recorded pre and postoperatively.
A patient is placed in prone position. An appropriate-sized elliptical graft is designed, so the longer diameter is placed in the gluteal skin groove. Dermal fat graft is harvested and prepared. Donor site is closed in layers with a running sutures. Then, patient is transferred in supine position. After subcoronal incision and penile degloving, dermal fat graft is shape adjusted, circumferentially equally placed and fixed along the penile shaft, between dartos and Buck’s fascia. Urethra is always left completely free. Ventral longitudinal incision with penile eversion and degloving is used in patients who request prepuce preservation. Penile skin reconstruction follows repair of dartos fascia.
Patient is discharged the next day after surgery. A compressive dressing is left in place for 7-10 days. Two weeks after surgery, patients should start using vacuum device twice a day (5-10 minutes) during the first six months to prevent temporary penile retraction. Patients can expect to achieve full result six to twelve months after surgery.
Our clinical experience with this treatment approach for penile girth enhancement showed its remarkable safety, excellent cosmetic results, low morbidity and low incidence of postoperative complications. Mean operative time is 90 minutes and final penile girth gain is approximately 3 cm. Erectile dysfunction or sensitivity deficiencies have not been reported so far in postoperative period. Patients may resume their sexual activity 6-8 weeks after surgical intervention.
CASE 1
 Penile girth is 7cm before surgery.
Penile girth is 7cm before surgery.
 Dermal graft is placed and fixed along the penile shaft, in circumference, using penoscrotal approach.
Dermal graft is placed and fixed along the penile shaft, in circumference, using penoscrotal approach.
 Appearance after surgery. Girth of the penile shaft is equally enhanced. Penis is not circumcised.
Appearance after surgery. Girth of the penile shaft is equally enhanced. Penis is not circumcised.

 Penile girth is 10cm after surgery.
Penile girth is 10cm after surgery.
CASE 2
 Preoperative appearance. A 15cmx4.5cm graft is designed in left gluteal region.
Preoperative appearance. A 15cmx4.5cm graft is designed in left gluteal region.
 Harvesting of the graft from the left buttock.
Harvesting of the graft from the left buttock.
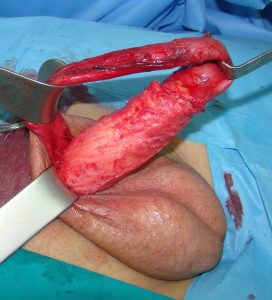
 Graft preparation.
Graft preparation.
 Closure of the wound. Drain is placed. The scar will remain hidden in the gluteal groove.
Closure of the wound. Drain is placed. The scar will remain hidden in the gluteal groove.
 Dermal graft is equally distributed and fixed to the penile shaft.
Dermal graft is equally distributed and fixed to the penile shaft.
 Appearance after surgery. Penopubic approach is used.
Appearance after surgery. Penopubic approach is used.
CASE 3
OUTCOME 4 WEEKS AFTER SURGERY



1. Djordjevic ML, Bumbasirevic U, Stojanovic B, Stevovic TK, Martinovic T, Bizic M, Kojovic V. Repeated penile girth enhancement with biodegradable scaffolds: microscopic ultrastructural analysis and surgical benefits. Asian J Androl. 2018 Sep-Oct;20(5):488-492.
2. Djordjevic ML. Penile enhancement surgery: challenges and limits. AJAM 2015: 55-8.
3. Djordjevic ML. Penile enhancement surgery. J Dtsch Dermatol Ges. 2010 Sep;8(9):645-7.
4. Perovic SV, Byun JS, Scheplev P, Djordjevic ML, Kim JH, Bubanj T. New perspectives of penile enhancement surgery: tissue engineering with biodegradable scaffolds. Eur Urol, 2006;49(1):139-47.
5. Perovic S, Djordjevic M, Kekic Z, Djakovic N. Penile surgery/reconstruction. Curr Opin Urol, 2002; 12:191-194.
6. Basting R, Perovic S, Djordjevic M, Djakovic N. Is real penile lengthening possible by simple ligamentolysis? Int J Impot Res, 2001; 13 (suppl.4): 22.
7. Perovic S, Djordjevic M. Penile lengthening. Br J Urol, 2000; 86: 1028-1033.
8. Perovic S, Djordjevic M, Djakovic N. Penile disassembly technique for real penile lengthening. J Urol, 1998; 159(Suppl. 5): 224.
9. Perovic S, Djordjevic M, Djakovic N. Penile lengthening: myth or reality. Eur Urol, 1998; 33(suppl 1): 153.
10. Perovic S, Djordjevic M, Djakovic N. Real penile enlargement. Br J Urol, 1997; 80(Suppl.2):308.
7. Basting R, Djakovic N, Djordjevic M, Perovic S. Surgical treatment of Peyronie’s plaque located under the glans cap using the penile disassembly technique and laser plaque treatment. Eur Urol, 2000; 37(suppl 2): 59.
8. Perovic S, Djordjevic M. Penile disassembly technique to surgical treatment of Peyronie’s disease. J Urol, 2000; 163(suppl.): 355.